For decades, treating diseases of the central nervous system (CNS) with stem cells has been hampered by one persistent biological obstacle: the blood–brain barrier (BBB).
While the BBB protects the brain from harmful substances, it also blocks most drugs and cell therapies, making the treatment of conditions like Parkinson’s disease, Alzheimer’s disease, and stroke extremely challenging. Traditionally, delivering stem cells directly to the brain has required invasive surgical procedures with inherent risks.
Research reviewed by Yu-Ting Zhang, Kai-Jie He, and colleagues at Soochow University highlights a noninvasive solution: delivering stem cells through the nose via intranasal administration (INA).



This technique, first demonstrated in animal models by William Frey in 1989 for small molecules and later for stem cells, allows cells and therapeutics to bypass the BBB, potentially transforming the landscape for nervous system repair.
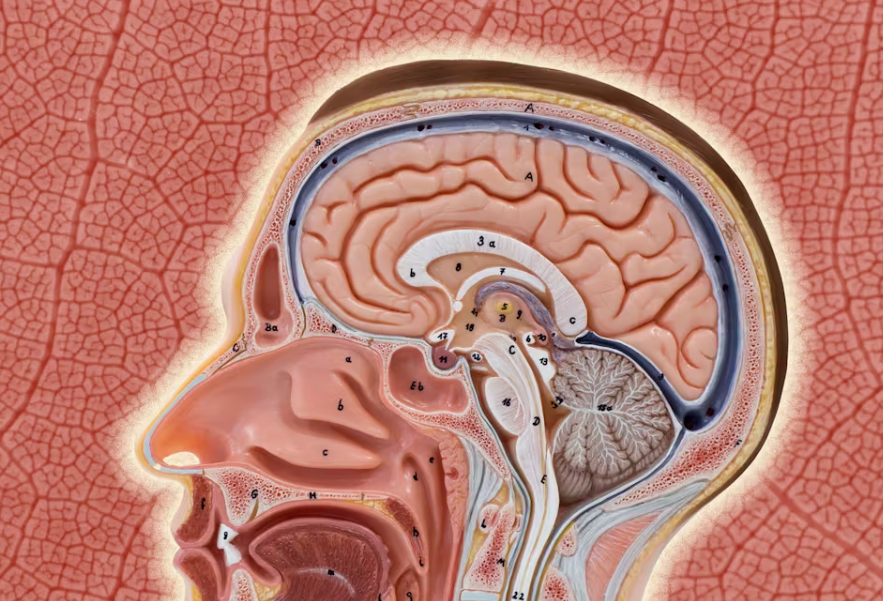
How Intranasal Delivery Gets Stem Cells to the Brain
What makes the nose such an effective gateway to the brain? Stem cells delivered intranasally can reach the CNS via several pathways:
- Olfactory and Trigeminal Routes: Substances deposited in the nasal cavity seem to travel along the olfactory and trigeminal nerves, accessing key brain structures (like the olfactory bulb, cortex, and brainstem) within minutes to hours.
- Perivascular and Cerebrospinal Fluid Spaces: Once past the nasal epithelium, stem cells may migrate through spaces surrounding blood vessels and the cerebrospinal fluid, facilitating distribution deep in the brain.
- Paracellular and Intracellular Pathways: The dynamic renewal of nasal epithelial cells creates temporary openings, and endocytosis by nerve cells can help internalize and transport cells across the nasal barrier.
Fluorescent labeling and advanced imaging in animal models in this study revealed that stem cells delivered this way can be found not just at entry points but also migrate to regions affected by injury or disease.
Stem Cell Types Used and Diseases Targeted
A variety of stem cell sources are being explored for intranasal delivery:
- Neural Stem Cells (NSCs): Able to become neurons or glia, NSCs show promise for treating neurodegenerative disorders and brain injuries.
- Mesenchymal Stem Cells (MSCs): Derived from bone marrow, fat, umbilical cord, and other sources, MSCs can protect or replace neurons and modulate inflammation.
- Induced Pluripotent Stem Cells (iPSCs): Engineered from adult cells to behave like embryonic stem cells, iPSCs may eventually solve immunogenicity and ethical concerns, though clinical use is still emerging.
Intranasal stem cell therapy has been studied in a range of preclinical CNS disease models:
- Parkinson’s Disease (PD): Intranasal MSCs and NSCs migrate to areas of neural degeneration, improve dopamine neuron survival, and ameliorate motor deficits in rodent models.
- Alzheimer’s Disease (AD): Intranasally delivered MSCs or their secreted factors reduce amyloid pathology and inflammation, showing beneficial behavioral effects in AD models.
- Stroke and Neonatal Brain Injury: Stem cells delivered by INA home to areas of ischemic injury and support tissue repair and functional improvement.
- Glioblastoma (GBM): NSCs delivered intranasally can target and persist near brain tumors, providing a platform for combination therapies, such as oncolytic viruses.

Advantages and Challenges of the Intranasal Route
Intranasal delivery offers several clear advantages over conventional routes:
- Noninvasiveness: It avoids the risks of stereotactic brain surgery or spinal injections.
- Targeted CNS Delivery: Higher CNS concentrations can be achieved without significant systemic exposure.
- Repeatability: Treatments can be administered multiple times, which may be necessary for chronic conditions.
- Reduced Side Effects: Other organs are spared from unnecessary exposure, potentially decreasing adverse events.
However, there are notable limitations:
- Efficiency: Only a fraction of the administered cells reach the brain. Most remain in the nasal cavity, and typically, only thousands of cells are detected in key brain regions after dosing millions.
- Migration and Engraftment: Not all stem cells distribute evenly, and their migration can vary by disease state, animal model, cell type, and age.
- Cell Type and Dosing: Studies are needed to clarify which cells work best and what dosing strategies optimize delivery and effect. Some evidence suggests that lower doses may sometimes work better than higher ones.
Further, while cell engraftment and survival in the brain are promising in animal models, confirming similar efficiency and safety in humans will require more research and clinical trials.
Moving Forward
The intranasal stem cell delivery route is a significant advance, potentially democratizing access to CNS regenerative therapies. Its greatest immediate promise may be for diseases that affect multiple brain areas or require repeated treatments, such as neurodegenerative disorders. Additionally, the use of stem cell-derived exosomes—small vesicles loaded with therapeutic factors—delivered intranasally is a rapidly growing area of interest, potentially sidestepping some of the challenges related to cell survival and migration.
The field now faces open questions about optimizing delivery, tracking cells in vivo, and translating these findings into effective, safe, and scalable treatments for patients. Nevertheless, the nose-to-brain route stands as one of the most promising and least invasive strategies for getting regenerative therapies where they are needed most: inside the protected environment of the human brain.
References Zhang YT, He KJ, Zhang JB, et al. Advances in intranasal application of stem cells in the treatment of central nervous system diseases. Stem Cell Research & Therapy. 2021;12:210. doi:10.1186/s13287-021-02274-0
This article summarizes peer-reviewed research and does not constitute medical advice. For questions on clinical application, consult a qualified healthcare professional.